Understanding Phlebitis Symptoms and Causes
Welcome to Truffles Vein Specialists, your trusted source for reliable information on vascular medicine, doctors, and health in the field of medical sciences. In this article, we will explore in detail the various symptoms and causes of phlebitis, shedding light on this vascular condition that affects numerous individuals worldwide.
What is Phlebitis?
Phlebitis, also known as vein inflammation, is a condition that occurs when a blood clot forms in a vein, causing inflammation and pain. This condition primarily affects the legs, although it can occur in other parts of the body as well. Understanding the signs and causes of phlebitis is crucial for early detection and proper treatment.
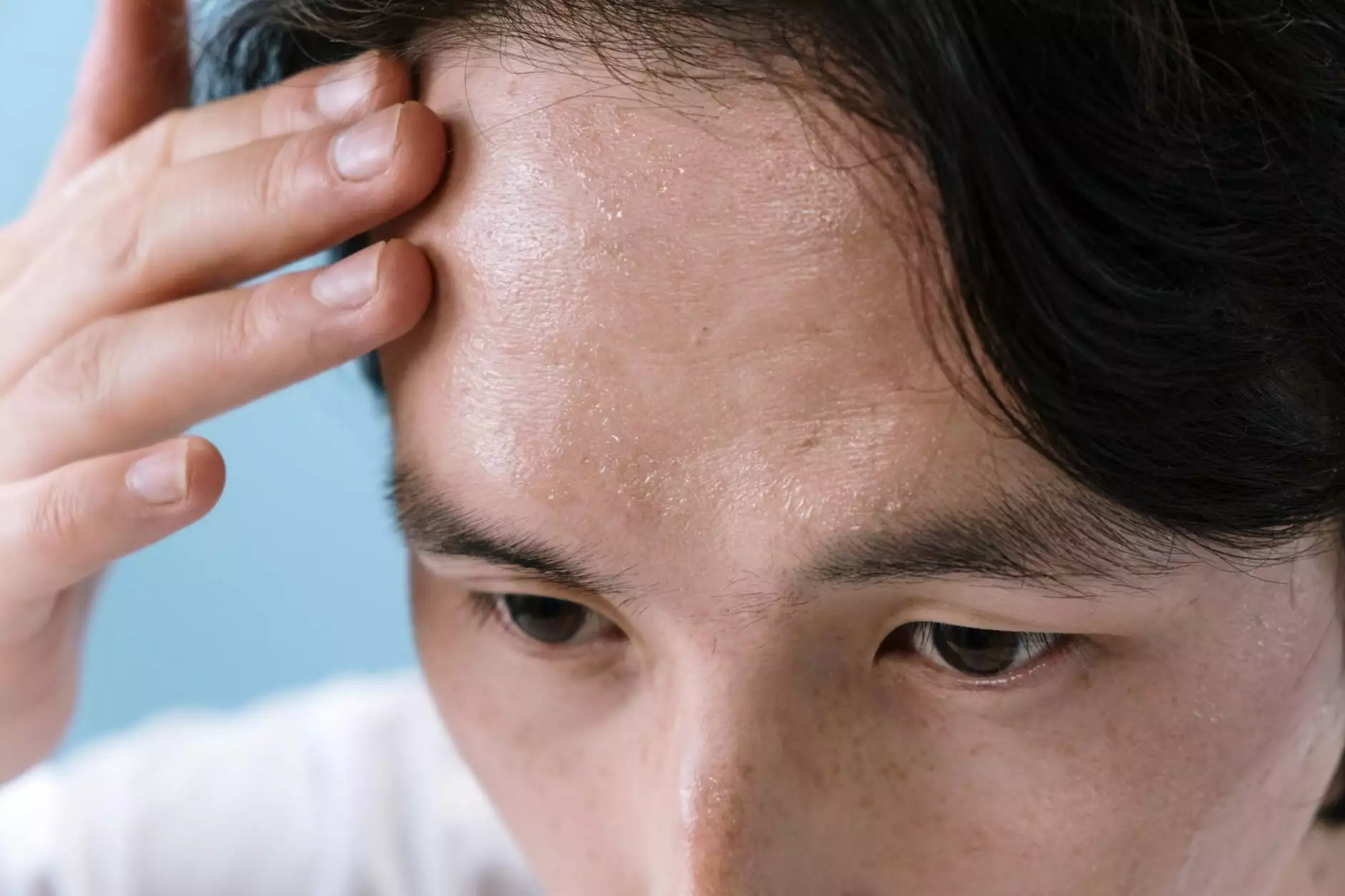
Common Symptoms of Phlebitis
Recognizing the symptoms of phlebitis is vital to seek medical attention promptly. The following are some common signs of phlebitis:
- Pain and tenderness: Individuals with phlebitis often experience pain and tenderness in the affected area. They may describe it as a throbbing or cramping sensation.
- Redness and warmth: The skin around the affected vein may appear reddish and feel warm to the touch. This is a visible indication of inflammation.
- Swelling: Swelling is another common symptom of phlebitis. It can range from mild to severe, depending on the extent of the clot and inflammation.
- Vein hardening: In some cases, the affected vein may feel hard or lumpy. This happens due to the clot and subsequent inflammation.
- Possible fever: In more severe cases of phlebitis, individuals may experience a mild fever or an overall feeling of illness.
If you notice any of these symptoms, it is essential to consult a doctor for a proper diagnosis and appropriate treatment.
Causes of Phlebitis
Various factors can contribute to the development of phlebitis. Understanding the underlying causes can help prevent its occurrence and manage the condition effectively. Here are some common causes of phlebitis:
1. Blood Clots:
Blood clots, also known as deep vein thrombosis (DVT), are a leading cause of phlebitis. These clots can form in the deep veins of the legs, restricting blood flow and causing inflammation. Certain medical conditions, such as obesity, pregnancy, and prolonged immobility, increase the risk of developing blood clots.
2. Trauma or Injury:
Phlebitis can also occur as a result of trauma or injury to the affected area. Mechanical damage to the vein can trigger inflammation and subsequent clot formation.
3. Medical Procedures:
Certain medical procedures, such as intravenous catheter insertion or frequent blood draws, can irritate the vein and lead to phlebitis. Individuals who require intravenous therapy or have chronic diseases that necessitate frequent blood tests are at a higher risk.
4. Infections:
Infections in the bloodstream can cause inflammation in the veins, leading to phlebitis. Bacterial or fungal infections, such as cellulitis or septicemia, are common culprits.
5. Underlying Medical Conditions:
Several medical conditions, including vasculitis, lupus, and Crohn's disease, increase the risk of developing phlebitis. These conditions affect the immune system or the veins directly, making individuals more prone to vein inflammation.
Effective Management of Phlebitis
Proper management of phlebitis involves a combination of medical intervention and lifestyle modifications. The following approaches are often recommended for phlebitis treatment:
1. Medication:
Your doctor may prescribe medications to alleviate pain, reduce inflammation, and prevent blood clot formation. Nonsteroidal anti-inflammatory drugs (NSAIDs) and anticoagulants are commonly prescribed.
2. Compression Therapy:
Wearing compression stockings or bandages provides external pressure on the affected area, promoting healthy blood flow and reducing swelling.
3. Elevation of the Legs:
Raising the legs above the level of the heart helps reduce swelling and improve circulation. Doctors often recommend keeping the legs elevated whenever possible.
4. Warm Compresses:
Applying warm compresses to the affected area helps alleviate pain and promotes blood flow. Be sure to follow your doctor's recommendations for duration and frequency.
5. Lifestyle Modifications:
Adopting a healthy lifestyle can significantly reduce the risk of phlebitis. Regular exercise, maintaining a healthy weight, avoiding prolonged sitting or standing, and quitting smoking are essential steps to prevent vein inflammation.
Remember, effective management of phlebitis requires personalized medical guidance. Consulting a specialist, such as the expert doctors at Truffles Vein Specialists, is crucial for accurate diagnosis, treatment options, and long-term care.
Conclusion
Phlebitis is a vascular condition that can cause discomfort and potentially serious complications if left untreated. Recognizing the symptoms and understanding the causes allow for early detection and prompt medical intervention. With the right treatment and lifestyle modifications, individuals with phlebitis can effectively manage this condition and improve their quality of life.
For further information, and to consult our renowned doctors specializing in vascular medicine, visit our website trufflesveinspecialists.com today. Take control of your vascular health and let our expertise guide you towards a healthier and happier life!
phlebitis symptoms and causes








